WHAT EVERY PARENT SHOULD KNOW BEFORE THEIR CHILD STARTS TESTOSTERONE THERAPY
By: Joy Stephenson-Laws, Holistic Coach, J.D., Founder
The conversation about long-term commitment, fertility, and the path back that most families never have.
When a young person begins testosterone therapy, families receive lists of expected benefits—more energy, better mood, improved strength. What they rarely receive is the complete picture of what a decade-long commitment to this hormone actually means for the body, for fertility, and for the very real possibility that stopping may not be simple.
This conversation matters because the decision to start isn't just about today. It's about every day that follows.
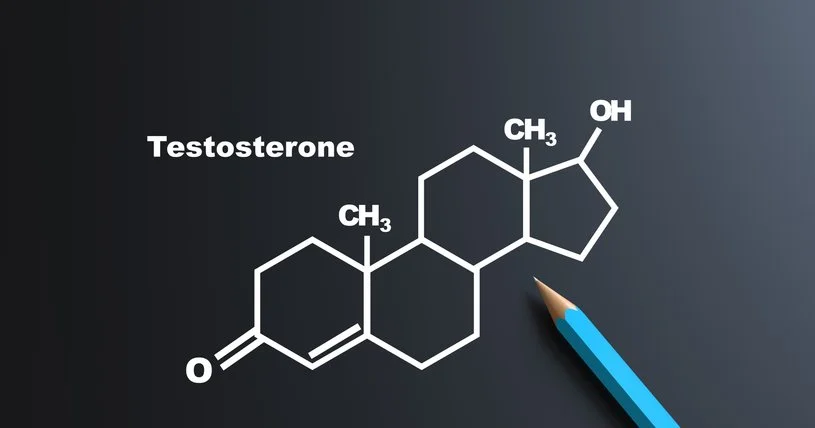
HOW TESTOSTERONE THERAPY CHANGES THE BODY
Your body operates on a feedback loop. Think of it like a thermostat. When the temperature reaches the set point, the heater turns off. Hormones work the same way.
When testosterone arrives from an outside source—gel, injection, or pellet—the brain receives a clear message: "We have enough. Stop making more." Within weeks, natural production begins to fade. The longer someone stays on outside testosterone, the more the body forgets how to make its own.
This isn't a side effect. This is how testosterone therapy works.
THE TRAUMA CONNECTION MOST DOCTORS MISS
Here's something that often surprises people: close to 80% of men with traumatic brain injury or PTSD have low testosterone. This isn't coincidence. The same systems that control testosterone are the ones disrupted by ongoing stress and trauma.
A child who experiences abuse lives in constant fight-or-flight mode. Their stress system stays activated for years. By the time they reach their teens or early twenties, they may show up with low testosterone, sluggish thyroid, anxiety, depression, and sometimes substance use to cope.
A doctor sees "low T" on the lab work and prescribes testosterone. The prescription helps—sometimes dramatically. But here's what often goes unsaid: the hormones are treating symptoms of trauma, not the trauma itself.
The testosterone isn't just replacing a missing hormone. For trauma survivors, it's functioning as part of their emotional regulation system, whether anyone names it that way or not.
THE FERTILITY QUESTION NO ONE ASKS
Research shows that up to 90% of men on testosterone therapy will have a significant drop in sperm count. Many become completely infertile while on treatment—sometimes within the first few weeks.
For teens and young adults, this creates a real problem. Many start therapy without understanding that their future ability to have biological children may be at stake. Any form of testosterone—gel, injection, or pellet—will lower sperm counts, often stopping production completely. The dose doesn't matter.
What many patients don't hear: this is a predictable consequence, not a rare side effect.
THE TEN-YEAR REALITY
For those on testosterone therapy for a decade or longer, the body has deeply adapted to receiving hormones from outside rather than making them inside. Research shows that both age and length of testosterone use affect recovery time. The longer the treatment, the less certain the return to normal function.
Extended therapy can cause testicular shrinkage, dependency (the body forgets how to work without it), and difficult withdrawal that can take 12 months or more to resolve.
Stopping isn't as simple as just ending treatment. Withdrawal symptoms can include crushing fatigue, depression, loss of muscle, and mental fog. For trauma survivors, stopping may bring back not just low-T symptoms but also PTSD-related hypervigilance and anxiety.
RECOVERY IS POSSIBLE—WITH THE RIGHT SUPPORT
Now for the part of this conversation that offers hope.
Consider someone who experienced childhood abuse, developed PTSD and hormonal problems, used substances to cope, and was prescribed testosterone at 21. On paper, this looks like a hard case for recovery after a decade of treatment.
But what if this person did the deeper work? What if they addressed the underlying trauma, got sober, learned to regulate their nervous system, and supported cellular healing through therapies like hyperbaric oxygen, PEMF, and red light therapy?
The picture changes completely.
The original reason for hormonal problems wasn't organ failure—it was trauma throwing everything off balance. If the trauma is healed, the nervous system is regulated, and substances are no longer causing damage, the body may now be capable of doing what it couldn't do at 21.
THE CELLULAR HEALING LAYER
Stopping testosterone after years of use asks the body to wake up systems that have been quiet and remember how to function. Medications like hCG and Clomid tell the body what to do. But the body also needs the cellular health and energy to actually do it.
This is where cellular healing therapies come in:
Hyperbaric Oxygen Therapy (HBOT) floods tissues with oxygen, activates stem cells, and reduces inflammation. Studies show testosterone levels increase after HBOT sessions.
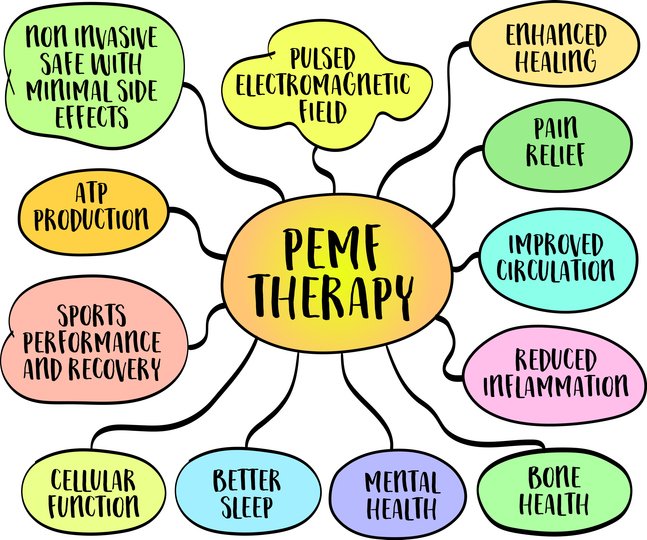
PEMF Therapy uses electromagnetic fields to calm inflammation, improve blood flow, and support the nervous system—including better sleep, which is when testosterone and growth hormone are made.
Red Light Therapy directly stimulates the Leydig cells that produce testosterone. Research shows it can increase testosterone by 70% in just two weeks and improve sperm motility without DNA damage.
Contrast Therapy (alternating hot and cold) reduces cortisol, which competes with testosterone production. The key: always end with cold to protect sperm quality.
Used together, these therapies create compounding benefits—reducing inflammation, energizing the cells that produce hormones, and keeping stress hormones from interfering with recovery.
THE QUESTIONS THAT MUST BE ASKED
For any young person considering testosterone therapy, these questions deserve honest answers before starting:
Has trauma history been explored? Could stress or adverse childhood experiences be contributing?
Would addressing the underlying cause resolve the hormone issue without medication?
Has sperm banking been discussed?
What's the exit strategy if they want to stop?
Would Clomid work instead? It raises testosterone without suppressing fertility.
Doctors often fail to tell patients about the risk of testosterone-induced infertility, partly because they don't know about it themselves. That must change.
FOR THOSE ALREADY ON LONG-TERM THERAPY
If you're reading this as someone who has been on testosterone therapy for years and is now concerned, know this: recovery is possible. The body is remarkably resilient.
With proper medical support—hCG, Clomid, peptides that help wake up the hormone system, and cellular healing therapies—most men can recover testosterone production and fertility. It takes time and patience. Give yourself 12-24 months.
The deeper work matters too. If your low testosterone was related to trauma, addressing those root causes will support your recovery and may mean you don't need testosterone therapy long-term.
THE BODY WANTS TO HEAL
True informed consent means knowing both the costs and the path back. When we provide this information clearly and compassionately, we honor the dignity of those making these decisions. We trust them to weigh the benefits against the risks. And we ensure that whatever choice they make is truly their own.
Your body wants to heal. The right support helps it remember how.
SUPPORTING RESEARCH
Fertility Recovery After Testosterone Therapy
Wenker EP, et al. "The Use of HCG-Based Combination Therapy for Recovery of Spermatogenesis after Testosterone Use." Journal of Sexual Medicine, 2015 — 95.9% of men showed return of sperm production with combination therapy.
World Health Organization Task Force meta-analysis: Sperm recovery to healthy levels in 67% within 6 months, 90% within 12 months, 100% within 24 months.
Kohn TP, et al. "Management of Male Fertility in Hypogonadal Patients on Testosterone Replacement Therapy." Medicina, 2024.
Trauma, PTSD, and Testosterone
"Stress, hypothalamic-pituitary-adrenal axis, hypothalamic-pituitary-gonadal axis, and aggression." Metabolic Brain Disease, 2024 — Documents the HPA-HPG axis interaction.
Shen H, et al. "Associations between testosterone and future PTSD symptoms." Translational Psychiatry, 2025.
"HPA axis function and diurnal cortisol in post-traumatic stress disorder: A systematic review." Neurobiology of Stress, 2019.
Hyperbaric Oxygen Therapy (HBOT)
Passavanti G, et al. "Can Hyperbaric Oxygenation Therapy Modify the Blood Testosterone Concentration?" Urologia, 2010 — Testosterone significantly increased after HBOT in both patients and healthy controls.
Zhang Y, et al. "Hyperbaric oxygen therapy for male infertility: a systematic review and meta-analysis." Asian Journal of Andrology, 2025 — HBOT improved sperm quality and fertility outcomes.
Pulsed Electromagnetic Field (PEMF) Therapy
Ross CL, et al. "The Use of Pulsed Electromagnetic Field to Modulate Inflammation and Improve Tissue Regeneration." Bioelectricity, 2021.
Kumar S, et al. "The therapeutic effect of a pulsed electromagnetic field on reproductive patterns." Clinics, 2011 — PEMF demonstrated protective effects against oxidative stress damage to reproductive tissues.
Red Light Therapy (Photobiomodulation)
Preece D, et al. "Red light improves spermatozoa motility and does not induce oxidative DNA damage." Scientific Reports, 2017 — 633nm light increased sperm swimming speed without DNA damage.
Fagiolini A, et al. University of Siena pilot study, 2016 — Light therapy increased testosterone from 2.1 to 3.6 ng/ml (70% increase) within two weeks.
Moskvin SV, Apolikhin OI. "Effectiveness of low level laser therapy for treating male infertility." Biomedicine, 2018.
Contrast Therapy
Podstawski R, et al. "Endocrine Effects of Repeated Hot Thermal Stress and Cold Water Immersion in Young Adult Men." American Journal of Men's Health, 2021 — Cortisol decreased significantly; testosterone increased ~5%.
Shefi S, et al. "Wet heat exposure: A potentially reversible cause of low semen quality." International Brazilian Journal of Urology, 2007 — Reducing hot water exposure improved sperm counts by ~500%.
Leonardi G, et al. "Mechanisms and Efficacy of Contrast Therapy for Musculoskeletal Painful Disease." Journal of Clinical Medicine, 2025.
Professional Guidelines
American Urological Association. "Evaluation and Management of Testosterone Deficiency: AUA Guideline." Journal of Urology, 2018.
Endocrine Society. "Testosterone Therapy in Men with Hypogonadism: Clinical Practice Guideline." Journal of Clinical Endocrinology & Metabolism, 2018.
This article is for educational purposes and does not constitute medical advice. Anyone considering starting or stopping testosterone therapy should work with qualified healthcare providers who can assess their individual situation.
Joy Stephenson-Laws is a healthcare attorney, certified holistic wellness coach, and founder of Proactive Health Labs. She is the author of "From Chains to Wings: A Poetry Revolution for Healing" and the children's book "Secrets That Sparkle (and Secrets That Sting)," which teaches children about emotional safety and the importance of trusted adults.