Trauma and Sleep Problems: Effective Strategies for Restful Nights
By Joy Stephenson-Laws, Holistic Coach, J.D., Founder
Because it’s not just your thoughts keeping you up—it’s your nervous system.
You’re exhausted. Your body says sleep, but your brain says nope.
Or maybe you do fall asleep, but wake up at 2:00 a.m. wired, panicked, or just… off.
If this sounds familiar, you’re not alone—and you’re not broken.
You’re likely dealing with sleep disruption that stems from trauma.
Let’s get into what that really means—and what you can do to finally get the kind of rest that heals.
1. Why Trauma Makes It Hard to Sleep
Sleep is vulnerable. To drift off, your body has to feel safe enough to surrender. But for people with unresolved trauma, that sense of safety can be hard to access—even if there’s no “danger” in the room.
Here’s what trauma can do to your sleep:
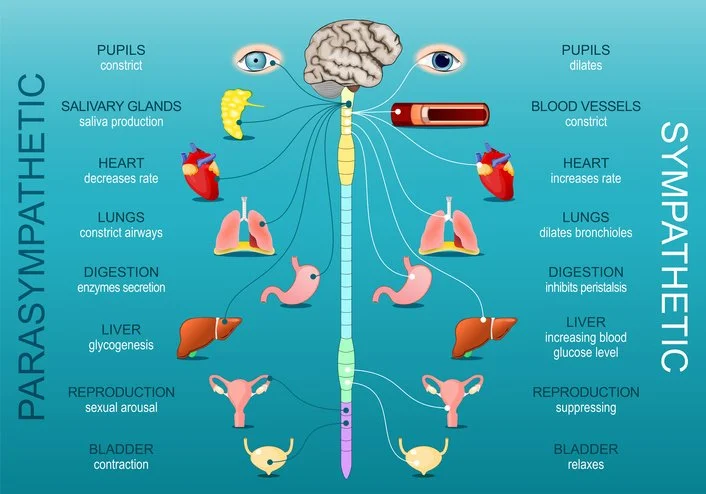
Keeps your nervous system in fight-or-flight
Elevates cortisol and reduces melatonin
Makes it hard to fall asleep—or stay asleep
Triggers nightmares, night terrors, or emotional flooding at night
Leads to waking up tired, groggy, or anxious despite hours in bed
2. Nightmares: Your Brain’s Night Shift
Nightmares aren’t random. They’re often the brain’s attempt to process emotional overload. If trauma hasn’t been fully metabolized, it can keep resurfacing in your dreams—especially during REM sleep.
Common themes:
Falling
Being chased
Losing control
Flashbacks or symbolic versions of trauma
For people with complex trauma or early developmental trauma, the dreams may be confusing but emotionally intense.
3. Not Sleeping = Still in Survival Mode
The sympathetic nervous system—the one responsible for survival—doesn’t clock out just because it’s dark outside. And if your system is stuck in high alert, you won’t drop into deep, restorative sleep.
Signs your body is still on defense:
Jaw clenching
Chest tightness
Waking with a jolt
Racing thoughts
Feeling tired but too wired to sleep
4. The Freeze State: Sleeping But Not Resting
Some trauma survivors fall asleep easily… but still wake up feeling like they ran a marathon in their dreams.
This may be dissociative sleep, where the body shuts down, but never fully relaxes. You sleep—but your nervous system never gets the memo that it’s safe.
This is especially common in:
Complex PTSD
People with a history of emotional neglect or chronic stress
Highly functional adults who’ve never stopped “performing”
5. Sleep Meds: Why They’re Not Always the Answer
It’s tempting to reach for something to “knock you out”—especially when you’re desperate. And while sleep medications (like Ambien, benzodiazepines, or over-the-counter aids) can help short-term, they may not be ideal for trauma-related sleep disruption.
Here’s why:
a. They Override, Not Regulate
Meds force the brain into unconsciousness, but don’t address the underlying hypervigilance or emotional distress. You sleep—but don’t truly rest.
b. They Disrupt REM Sleep
Many sleep aids reduce or suppress REM sleep, which is where emotional processing happens. So you may sleep… but not heal.
c. Dependence and Rebound Insomnia
Long-term use can lead to tolerance, dependency, or worse sleep when you try to stop.
d. They Mute the Message
Insomnia can be your body’s way of saying, “There’s something here I need to feel or heal.” Sleep meds quiet the symptom but not the story.
6. The Gut-Sleep-Trauma Triangle
Your gut produces most of your serotonin, which becomes melatonin, your sleep hormone. Trauma messes with your gut (remember the reflux and diarrhea?), which means it can also mess with your sleep cycle.
Dysbiosis = mood swings and low serotonin
Low serotonin = less melatonin
Less melatonin = can’t fall or stay asleep
A trauma-informed sleep approach includes gut support, too.
7. How to Support Healing Sleep (Without Forcing It)
Here’s what actually helps trauma survivors sleep better over time:
a. Create a “Safety Ritual” at Night
Instead of just a sleep routine, try a nervous system routine:
Weighted blanket
Candlelight
Aromatherapy (lavender, cedar, vetiver)
Guided meditations (especially Yoga Nidra)
b. Long Exhales, Longer Sleep
Try 4-7-8 breathing or coherent breathing (inhale 4, exhale 6) to downshift the nervous system into rest-and-digest mode.
c. Journaling Before Bed
If your thoughts keep spinning, write them down. This tells your brain, “We’ve offloaded. You’re safe to rest now.”
d. Trauma-Informed Somatic Work
Practices like TRE (Tension & Trauma Releasing Exercises), EMDR, or somatic experiencing can help unwind stored survival energy.
e. Nutritional Support
Magnesium glycinate or L-threonate
Herbal allies like passionflower, lemon balm, and reishi
Avoid sugar, alcohol, and caffeine within 6 hours of bedtime
f. Consider Professional Help
Trauma-focused CBT or EMDR therapy is proven to improve sleep, even in long-standing insomnia.
Final Thought: Rest Is a Birthright—Not a Luxury
If you can’t sleep, your body is not betraying you. It’s protecting you.
The solution isn’t to “shut it down”—it’s to listen, regulate, and rebuild trust with your nervous system.
True rest doesn’t start with sleep. It starts with safety.
When your body believes it can let go, sleep will return.
Not just as escape—but as a homecoming.
References and Recommended Reading
1. Lancel, M., van Marle, H. J. F., Van Veen, M. M., & van Schagen, A. M. (2021, November 24). Disturbed sleep in PTSD: Thinking beyond nightmares. Frontiers in Psychiatry, 12, Article 767760.
2. Zhang, Y., Lang, R., Guo, S., Luo, X., Li, H., Liu, C., Dong, W., Bao, C., & Yu, Y. (2022). Intestinal microbiota and melatonin in the treatment of secondary injury and complications after spinal cord injury. Frontiers in Neuroscience, 16, 981772.
3. Talbot, L. S., Maguen, S., Metzler, T. J., Schmitz, M., & McCaslin, S. E. (2018). Cognitive behavioral therapy for insomnia in post‑traumatic stress disorder: A randomized controlled trial. Journal of Clinical Sleep Medicine, 14(7), 1067–1077.
4. Qaseem, A., Kansagara, D., Forciea, M. A., Cooke, M., & Denberg, T. D. (2016, July 19). Management of chronic insomnia disorder in adults: Clinical practice guideline from the American College of Physicians. Annals of Internal Medicine, 165(2), 125–133.
5. Talbot, L. S., Maguen, S., Metzler, T. J., Schmitz, M., McCaslin, S. E., Richards, A., ... & Neylan, T. C. (2018). Cognitive behavioral therapy for insomnia reduces fear of sleep and associated PTSD symptoms. Journal of Clinical Sleep Medicine, 14(4), 683–692